- Review
- Open access
- Published:
Willingness to join community-based health insurance and associated factors among households in Ethiopian: a systematic review and meta-analysis
Cost Effectiveness and Resource Allocation volume 23, Article number: 12 (2025)
Abstract
Background
In Ethiopia, out-of-pocket medical expenses make up one-third of all medical expenses, which makes it difficult for households to obtain and utilize healthcare. One of the prepayment mechanisms that shield low-income households from unaffordable medical bills is the community-based health insurance (CBHI) program. This systematic review and meta-analysis aimed to estimate the pooled willingness to join Community-based Health Insurance schemes and its associated factors among households in Ethiopia.
Methods
Articles were searched from PubMed, Google Scholar, Web of Science, Scopus, Science Direct, and Ethiopian Universities’ repositories for grey literature. The study used the modified PRISMA guidelines for rewriting and reviewing the literature. The quality of studies was assessed using Joanna Briggs Institute Critical Appraisal tools. Data was extracted using Microsoft Excel and exported to STATA version 16 software for analysis. Cochran’s Q statistic and I2 tests were utilized to determine the heterogeneity between studies. Studies publication bias was determined using a funnel plot and Egger’s test. Subgroup analysis was conducted to demonstrate variations of the effect sizes across study regions. Finally, we utilized a random-effect model to compute the overall willingness to join the CBHI scheme and its determinants among households in Ethiopia.
Result
We included thirty studies to determine the pooled prevalence of willingness to join the CBHI scheme and its determinants. The pooled magnitude of households’ willingness to join the CBHI scheme was 60.42% (95% CI: 51.45%, 69.38%). Old aged (AOR = 2.17, [95% CI: 1.37, 3.44], I2 = 82.33%), formal educational status(AOR = 2.74, [95% CI: 2.10, 3.56], I2 = 59.85%), Rich wealth index (AOR = 2.51, [95% CI: 1.99, 3.18], I2 = 48.25%), good knowledge/awareness of CBHI scheme(AOR = 4.21, [95% CI: 3.01, 5.88], I2 = 66.0%), experienced illness in the last three months (AOR = 3.42, [95% CI: 2.19, 5.35], I2 = 71.15%), and large family size (AOR = 2.36, [95% CI: 1.95, 2.87], I2 = 50.81%) were determinants of willingness to join the CBHI scheme. In addition, affordability of CBHI premium (AOR = 3.12, [95% CI: 2.34, 4.14], I2 = 10.35%), poor health status (AOR = 3.23, [95% CI: 2.57, 4.06], I2 = 35.97%), trust in scheme (AOR = 4.38, [95% CI: 1.91, 10.06], I2 = 88.35%), chronic diseases (AOR = 3.24, [95% CI: 2.40, 4.37], I2 = 67.15%) and good quality of healthcare services (AOR = 2.91, [95%CI:2.08, 4.09], I2 = 65.40%) were also predictors of willingness to join the CBHI program.
Conclusion
The pooled prevalence of willingness to join the CBHI scheme was low and below the national target of 80%. Age, family size, educational status, wealth status, illnesses in last three months, presence of chronic illnesses, affordability of the premium for the CBHI scheme, self-reported health status, Knowledge/awareness of the scheme, trust in the scheme and perceived quality of healthcare service were significantly determine the willingness to join the CBHI scheme. Health providers should provide detailed awareness creation through health education on the concepts and principles of the CBHI scheme.
Introduction
Approximately 200 million people worldwide experience catastrophic health costs each year, with over 90% of these cases occurring in low- and middle-income countries (LMICs) [1]. Due to the low coverage of prepayment methods and underfunded public health systems in LMICs, out-of-pocket payments (OOP) have been a means of paying for medical services for the past ten years [2]. High OOP medical expenses were a major challenge in achieving universal health coverage (UHC) for sub-Saharan African(SSA) Countries including Ethiopia [3, 4]. In Ethiopia, OOP expenses for households make up one-third of all medical expenses, which makes it difficult for households to obtain and utilize healthcare [5].
To overcome financial hardship during service delivery, the government introduced prepayment modalities [6]. The community-based health insurance (CBHI) is a voluntary type of health insurance designed to shield low-income households from unaffordable medical bills, which is a part of the 2005 healthcare finance reform and receives significant government subsidies [7, 8]. After the reform, the CBHI program became a popular way to increase the health expenditures per capita, healthcare utilization, and health facilities service qualities in Ethiopia [8,9,10,11,12]. Although the CBHI scheme is crucial in avoiding financial hardship and improving healthcare quality in Ethiopia, the use of such strategies has been limited by the low coverage of the program [7]. The households’ willingness to join the CBHI scheme varies from region to region. For instance, the household enrollment rate was 73%, in the West Arsi zone [13], 78%, in the Bench Maji zone [14], and 12.8%, in the Sidama zone [15]. Socioeconomic factors (i.e. age, sex. Education, occupation, income, and family size), health and health-related factors (distance to facilities, health status, chronic illness, illnesses in family members, and quality of healthcare), CBHI-related factors (affordability of premiums, trust of households’ towards CBHI premium management, knowledge, and attitude towards CBHI program) were found to determine the CBHI scheme uptake [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39].
In Ethiopia, comprehensive evidence of households’ level of willingness to join the CBHI scheme is still needed using a systematic review and meta-analysis from primarly studies to amend insurance policies and decide on the program at the national and regional levels. There are two published studies which assessed the pooled uptake of the CBHI scheme in Ethiopia after our review was submitted for publication. The first systematic reviews and meta-analysis conducted by Tahir et al. [40] included 17 studies published from 2016 to 2020 to determine the pooled coverage of community-based health insurance scheme enrolment in Ethiopia. However, this review missed important studies [13, 16, 25, 28, 31, 33,34,35,36] on CBHI enrolment and used a magnitude from case-control studies [18] to determine the pooled magnitude of CBHI uptake. In addition, this systematic review and meta-analysis included studies done on dropout rate/membership renewal [41, 42], compliance [43], and the impact of CBHI on healthcare utilization and quality of life [44,45,46] to determine the pooled CBHI enrolment in Ethiopia. Thus, the studies dealing with dropout rate, membership renewal, the effect of CBHI on healthcare utilization, and compliance with a requirement of the CBHI scheme must be treated as unreliable sources of evidence for pooled CBHI uptake. In our review, we selected the dropout rate/membership renewal studies in the review only when they also dealt with CBHI uptake or enrolment as outcome variables. Besides, the recent systematic review and meta-analysis done by Habte et al. [47] included 15 studies published from 2017–2022(11 Cross-sectional and 4 Case-control) to determine the pooled magnitude of CBHI enrolment in Ethiopia. However, this study also missed pertinent studies [13, 16, 21, 24, 28, 30, 31, 33, 34, 36] while synthesizing evidence on CBHI uptake which might undermine the national figure to some extent. Thus, our systematic review and meta-analysis aimed to fill the above-mentioned gap and planned to determine the pooled magnitude of households’ willingness to join the CBHI scheme and its determinants in Ethiopia.
Method and material
Protocol registration and reporting
The preferred reporting items for systematic review and meta-analysis (PRISMA) 2020 guidelines were followed for rewriting and reviewing the literature [48]. The protocol of this systematic review and meta-analysis was registered at PROSPERO databases and available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022304861.
Search strategy
Both published and unpublished articles were searched in PubMed/Medline, Google Scholar, Web of Science, Science Direct, Scopus, and Ethiopian Universities’ repositories from January 31, 2022 to March 28, 2022. Medical Subject Heading (MeSH) and keywords such as (“Willingness to join“[All Fields] OR “enrolment“[All Fields] OR “adoption“[All Fields] OR “Uptake“[All Fields] OR “participate“[All Fields] OR “utilization“[All Fields]) AND (“community-based health insurance“[All Fields] OR “Community Health Insurance“[All Fields] OR “health insurance“[All Fields] OR “Mandatory Health Insurance“[MeSH Terms]) AND (“Ethiopia“[MeSH Terms] OR “Ethiopia“[All Fields])” combined with boolean operators were utilized to retrieve relevant studies from the electronic database (S1). Likewise, the authors retrieved a few relevant articles by searching the reference lists of included studies that might have been omitted during electronic database searching.
Eligibility criteria
Inclusion criteria
The review included both published and unpublished observational (Cross-sectional and case-control) studies conducted in Ethiopia, articles published in English, and studies performed since 2010 were considered. In addition, we used condition, context, population, and exposure of interest (CoCoPop/PEO) to frame the eligibility criteria. Population: included urban or rural Households, whereas exposure of interest included determinants factor that affects households’ level of willingness to join the CBHI scheme in Ethiopia. Condition/outcome: The primary outcome of the study includes Households’ willingness to join CBHI, defined as the motivation for heads of households to enroll in voluntary health insurance to benefit from the program, regardless of the payment, and is assessed using closed-ended binary questions after the principle and concept of the scheme are explained. The determinants of household willingness to join the CBHI scheme were the secondary outcome, measured using odds ratio (OR) and calculated based on the odds ratio and 95% Confidence Interval(CI) from primary studies included in the analysis. Secondary outcomes include socioeconomic factors (age, wealth index, educational status, and family size); environmental factors (travel time or distance to health facility); and health and health-related factors (self-reported health status, chronic illness, or any illness in the last three months and perceived quality of healthcare), the CBHI related factors (premium affordability, participation in solidarity organization, knowledge, and attitudes towards the CBHI scheme).
Exclusion criteria
Studies conducted in other than English languages, did not report outcomes for willingness to join the CBHI scheme, were not fully accessible, had methodological problems, editorial, qualitative studies, case reports, conference reports, reviews, commentary, letters, and studies done outside of Ethiopia were excluded from the study.
Study selection
We used the PRISMA reporting guidelines to screen the retrieved articles and select the relevant studies. Duplicated articles were removed using EndNote reference manager software version X7. Then, two reviewers (AWK and HEH) assessed the retrieved articles for title and abstract, and irrelevant titles and abstracts were removed. Finally, the remaining articles were reviewed for the full-length texts against the selection criteria. Disagreements between two reviewers during the study selection process were resolved by discussion with a third reviewer (BGD).
Data extraction
Two Reviewers (AWK and HEH) independently extracted data for each included article using a data abstraction format designed in Microsoft Excel. For each article, the authors extracted the following information: study design, region, publication year, sample size, response rate, the magnitude of willingness to join the CBHI scheme, and its associated factors. We developed the abstraction form containing the Odds ratio and 95% CI for extracting the determinants of willingness to join the CBHI scheme. In this systematic review and meta-analysis, we included the determinants of households’ willingness to join the CBHI program if they were reported as determinants in at least four studies.
Quality assessment
An essential component of systematic reviews and meta-analyses is critical appraisal, which assesses the quality of published articles, descriptions, reporting standards compliance, internal validity, and analysis methodology. Joanna Briggs Institute’s (JBI) quality check tool for observational studies was used to appraise the quality of each study. The JBI quality appraisal checklist for prevalence and case-control studies has nine and ten parameters, respectively [49, 50]. Two reviewers (AWK and HEH) independently assessed the quality of each study. The reviewers provided a score of ’1’ if the study met each specific parameter and ‘0’ if not the case. Next, using the JBI criteria to determine the risk of bias, the scores were computed, translated to percentage, and classified as poor quality/high risk of bias (≤ 49%), moderate quality/moderate risk of bias (50–69%), and excellent quality/low risk of bias (≥ 70%) [51, 52].
Data analysis
Relevant data were extracted using Microsoft Excel and imported into STATA 16 for analysis. Cochran’s Q-statistic and I2 statistics were used to assess the heterogeneity of the included papers; I2 values of 25%, 50%, and 75%, respectively, indicate low, moderate, and high heterogeneity [53, 54]. Leave-one-out sensitivity analyses were used to determine the source of heterogeneity among studies. The pooled prevalence of households’ willingness to join the CBHI scheme was estimated using random effect meta analysis because the included studies have high heterogeneity. The determinants of households’ willingness to join the CBHI scheme were reported using pooled odds ratio with 95% confidence intervals. Sub-group analysis by region was also done to present the variation in the level of willingness to join the CBHI program across study areas. The presence of publication bias was checked using Egger’s tests at a 5% significant level and by visual inspection of the funnel plot for the symmetry of the study heterogeneity. Lastly, the pooled estimates for willingness to join the CBHI scheme and its determinants were displayed using forest plots along with the appropriate 95% confidence intervals.
Result
Study selection
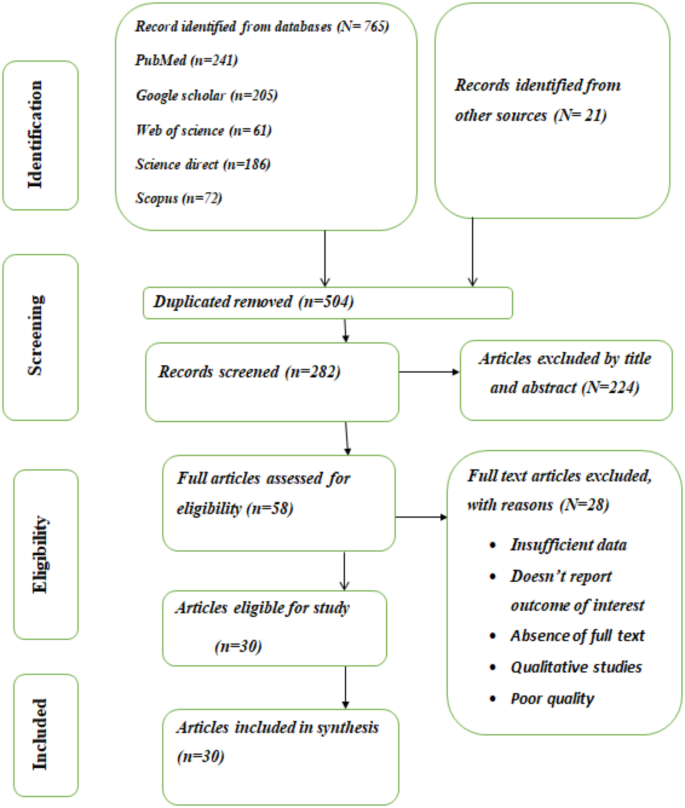
A total of 786 records were identified from electronic databases and other sources, out of which 504 were duplicated. After excluding duplicated studies, 224 studies were further removed based on titles and abstracts, and 58 full-text articles remained. After rigorous screening of the remained full-text articles based on eligibility criteria, 28 records were removed. The criteria for exclusion of the full-text articles include studies with insufficient data, methodological problems, reviews, that didn’t define the outcome of interest appropriately, qualitative studies, poor quality studies, and studies conducted outside of Ethiopia. Finally, we found 30 studies (24 cross-sectional and 6 case-controls) were eligible for the final systematic review and meta-analysis (Fig. 1).
Characteristics of included study
This systematic review and meta-analysis included thirty (24 cross-sectional and 6 case-control) studies for final analysis and synthesis. The review includes eleven studies from Amhara [17, 18, 20, 24, 27, 28, 30, 31, 36, 39, 55], and eleven studies from Oromia [13, 16, 21, 22, 25, 29, 32,33,34,35, 56], and four studies from the SNNPR region [14, 15, 19, 26] and two studies from Addis Ababa city [23, 38] and one studies from Somali [37] and Benishangul Gumuz [57]. The included studies were done between 2014 and 2022 and a majority (18/30) of them were published after 2019. The sample sizes of the studies varied from 216 to 2008, with a total sample size of 18,739 (Table 1).
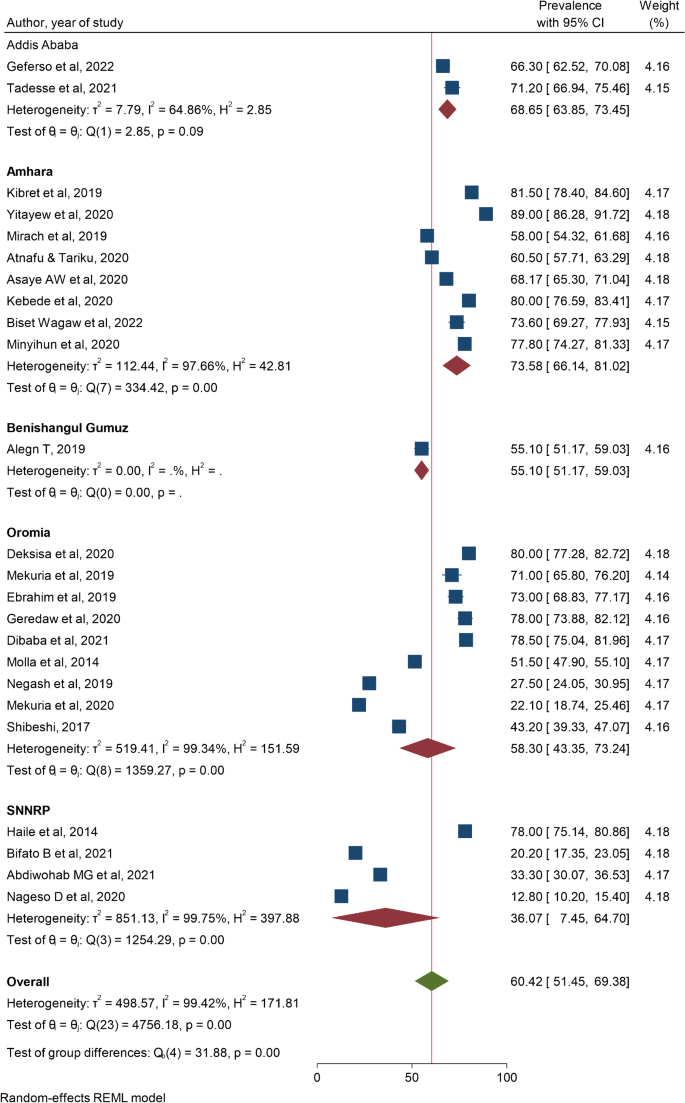
Prevalence of households’ willingness to join the CBHI scheme in Ethiopia
Out of 30 studies, 24(twenty-four) of them were used to compute the pooled prevalence of willingness to join the CBHI scheme. The I2 statistics result showed a high heterogeneity for the study (I2 = 99.17%, P-value < 0.01). Therefore, a random-effect model with a DerSimonian and Laird random method was used to determine the pooled prevalence of willingness to join the CBHI scheme in Ethiopia. Meta-analysis of 24(twenty-four) studies revealed that the pooled prevalence of willingness to join the CBHI program among households in Ethiopia was 60.42%(95%CI:51.45,69.38) [13,14,15,16,17, 19,20,21, 23,24,25,26, 28,29,30,31, 33,34,35,36, 38, 39, 56, 57]. We found the highest willingness to join the CBHI scheme in the study done in Simada District, Ethiopia, 89% [28], and the lowest willingness to join the CBHI scheme was observed in Sidama Zone (12.8%) [15] (Fig. 2).
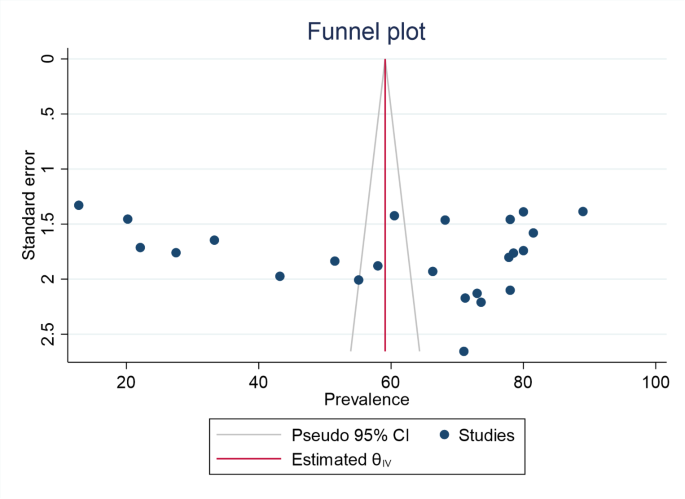
Publication bias
By visually inspecting the symmetry Funnel plot of the included papers and applying Egger’s and Begg’s tests, we evaluated the possibility of publication bias. The included studies were distributed symmetrically, and the visually examined funnel plot demonstrated that there was no publication bias. We also conducted Eggers-Egger’s and Begg’s tests, which yielded p-values of P = 0.332 and P = 0.823, respectively, and revealed no indication of a small-study effect (Fig. 3).
Subgroup analysis
We performed the subgroup analysis to compare the willingness to join the CBHI scheme across study areas. The finding showed that the overall willingness to join the CBHI scheme was higher in Amhara [73.58%, 95% CI: (66.14–80.02%)] [17, 20, 24, 28, 30, 31, 36, 39] while the lowest pooled prevalence of willingness to join the CBHI scheme was found in SNNPR[36.07%, 95% CI: (7.45–64.07%)] [14, 15, 19, 26] (Fig. 4).
Sensitivity analysis
Table 2 shows the willingness to join the CBHI scheme sensitivity analysis for every study that omitted one at a time. A leave-one-out sensitivity analysis was carried out on willingness to join the CBHI scheme among households in Ethiopia to pinpoint the possible cause of the analysis’s variability. We discovered that no single study had an impact on the households’ overall willingness to join the CBHI scheme(Table 2).
Determinants of households’ willingness to join the CBHI scheme in Ethiopia
In this systematic review and meta-analysis, we included 30 primary studies to investigate the pooled prevalence of willingness to join the CBHI programs and its determinants in Ethiopia. The odds of households’ willingness to join the CBHI program among old-aged households were almost two (AOR 2.17, [95% CI: 1.37, 3.44], I2 = 82.33%), p < 0.001 times higher than in young households. The households whose family size was ≥5 were 2.36 times more likely to join the CBHI scheme than their counterparts (AOR 2.36, [95% CI: 1.95, 2.87], I2 = 50.81%), p < 0.001. The random effect of the meta-analysis found that respondents with formal education were 2.74 times more likely to participate in the CBHI program than their counterparts (OR = 2.74, 95%CI: 2.10, 3.56], I2 = 59.85%). Households with a rich quintile wealth index were approximately three times more likely to join the CBHI scheme than their counterparts (AOR = 2.51, [95%CI:1.99–3.18], I2 = 48.25%).
Households that had poor health status had 3.23 times higher odds of joining the CBHI scheme than those that had good self-reported health status (OR = 3.23, [95% CI: 2.57, 4.06], I2 = 35.97%). The odds of households who encountered illnesses in the last three months were almost 3.42 times higher compared to their counterparts (AOR = 3.42, [95% CI: 2.19, 5.35], I2 = 71.55%). Households that had chronic illnesses were 3.24 times more likely to join the CBHI scheme than those that had no underlying diseases (AOR = 3.24, [95% CI: 2.40, 4.37], I2 = 67.15%).
The likelihood of joining the CBHI scheme was 2.91 times higher among participants who perceived that public healthcare quality is good compared with their counterparts (OR = 2.91, [95% CI: 2.08, 4.09], I2 = 65.40%). In addition, respondents who could afford the CBHI scheme premium had 3.12 higher odds of joining the CBHI scheme than those who could not afford it (AOR: 3.12, [95% CI: 2.34, 4.14], I2 = 10.35%). Moreover, households who had trust in the CBHI scheme were 4.03 times more likely to join the CBHI program than their counterparts (OR = 4.38, [95% CI: 1.91, 10.06], I2 = 88.35%). Furthermore, respondents who had good knowledge of the CBHI program were almost four times more likely to join the CBHI scheme than those who had poor knowledge of the CBHI scheme (AOR = 4.21, [95% CI: 3.01, 5.88], I2 = 66.0%), p < 0.001(Table 3).
Discussion
World Health Organization recommended countries should implement prepayment mechanisms to achieve UHC and overcome catastrophic financial costs for health service users [33]. Community-based health insurance schemes are the best to protect poor households against catastrophic healthcare expenditures [7]. This systematic review and meta-analysis intended to estimate the pooled prevalence of households’ willingness to join the CBHI scheme and its determinants in Ethiopia. The pooled prevalence of households’ willingness to join the CBHI scheme in Ethiopia was 60.42% (95%CI: 51.45, 69.38). This finding is almost comparable with the study conducted in Nigeria, 59.4% [58], and Kenya, 62% [59]. However, this finding is higher than the study conducted in Cameron, 46% [60], Uganda, 44% [61], and Kenya, 46% [62] and lower than the findings of a study done in Nepal, 88% [63], Nigeria, 90% [64], Enugu State, Nigeria, 92.4% [65], and the national coverage target, 80% [7]. The reason for the discrepancy might be due to the study period, study area, level of awareness about the CBHI scheme as well as the perception of participants towards the CBHI scheme.
The meta-analysis revealed that the old-aged respondents were more likely to join the CBHI program than young individuals. This finding is consistent with the findings of previous studies [66, 67]. This is explained by the fact that older groups are prone to illnesses and visit health facilities frequently for diseases that may expose them to financial hardship. Thus, this will encourage older age groups to join the CBHI to cover their healthcare costs during their illness. The study also found respondents who attended formal education had higher odds of joining the CBHI scheme than their counterparts. This finding is supported by previous meta-analyses [65, 68, 69], which showed education is positively associated with households’ willingness to join the CBHI scheme. This might be explained by the fact that educated households have a better understanding of the principles and benefits packages of the CBHI program in addition to their good know-how regarding the benefit of joining the CBHI program to overcome catastrophic health expenditure. In addition, the meta-analysis showed that households with larger family sizes were more likely to join the CBHI program than households with smaller family sizes. This finding is similar to the findings of previous studies [68,69,70]. This is because respondents with large family sizes might face a higher risk of illnesses and suffer from financial risks, particularly in poor communities. So, they prefer to join the CBHI scheme to avoid the risk of catastrophic out-of-pocket payment during the time of illness. Furthermore, households with a rich wealth index had higher odds of joining the CBHI scheme than those who had a poor wealth index. This finding is supported by previous systematic and meta-analyses [68,69,70] which reported income as a significant determinant of willingness to join the CBHI scheme. This is explained by the fact that individuals who have a rich wealth index can afford the CBHI scheme contribution at any price.
This meta-analysis found that households who experienced illnesses in the last three months had higher odds of joining the CBHI program compared to their counterparts. This evidence is supported by findings from previous studies [68, 70, 71]. This study also revealed that households who reported poor health status were more likely to join the CBHI scheme compared with their counterparts. This finding is in line with the study done by Bayked et al. [70] and Dror et al. [68]. This is because individuals who have poor health status experience more illnesses and visit public health facilities frequently which might expose them to catastrophic out-of-pocket healthcare expenditure that increases their probability to join the CBHI scheme. Besides, this meta-analysis showed that households who had chronic illnesses had higher odds of joining the CBHI program than those who had no underlying disease. This finding is consistent with the report of the studies [68, 70, 71]. This is explained by the fact that respondents with underlying diseases had frequent visits for follow up which exposed them to financial risk that forced them to join the CBHI scheme. Furthermore, the Meta-analysis revealed households who perceived the quality of healthcare services as good were more likely to join the CBHI scheme than their counterparts. This finding is supported by the Meta-analysis in LMICs [66,67,68, 70, 71], which reported quality of healthcare as facilitators of CBHI uptake. This might be due to the presence of good quality of healthcare in public health assists the households to get effective and efficient services that motivate them to join the CBHI scheme.
In this systematic review and meta-analysis, we found that households who perceived CBHI premium as affordable were more likely to join the CBHI scheme compared to their counterparts. This finding is concurrent with the previous studies [68, 71], which found affordability of the CBHI contribution is positively associated with CBHI uptake. The study also found household heads who trust scheme management had a higher likelihood of joining the CBHI scheme than those who did not trust the scheme management. This report is in line with the findings of the previous systematic review and meta-analysis [66, 67], which found trust in CBHI scheme management as facilitators of enrolment in the program. In addition, this meta-analysis points out that the households who good knowledge/awareness were more likely to join the CBHI scheme compared to their counterparts. Previous systematic reviews and meta-analyses [66,67,68, 70] also reported having knowledge/awareness of the CBHI scheme was positively associated with enrolment in the CBHI scheme. This might be because individuals who had awareness of the CBHI scheme principle and concept understand the advantage of joining the CBHI scheme. Our study has several limitations. Firstly, we didn’t get data from all regions of the country and this might affect the representativeness of our study. Secondly, Our pooled CBHI uptake had to be compared with primary studies from other countries because there were no meta-analysis studies on the willingness to join the CBHI program at the global or continental level. Thirdly, the difference in the categorization of some study variables was a great challenge during conducting pooled odds ratio to assess the determinants of the CBHI scheme uptake.
Conclusion
The pooled prevalence of willingness to join the CBHI scheme was low and below the national target of 80%. Age, family size, educational status, wealth status, illnesses in last three months, presence of chronic illnesses, affordability of the premium for the CBHI scheme, self-reported health status, Knowledge/awareness of the scheme, trust in the scheme and perceived quality of healthcare service were significantly determine the WTJ the CBHI scheme. Health providers should provide detailed awareness creation through health education on the concepts and principles of the CBHI scheme. In addition, leaders in health sectors should give attention to improving the health service quality.
Data availability
Data will be made available by request.
Abbreviations
- CBHI:
-
Community-based Health Insurance
- CI:
-
Confidence Interval
- LMIC:
-
Low to Medium-Income Countries
- JBI:
-
Newcastle-Ottawa Scale
- OR:
-
Odd Ratio
- UHC:
-
Universal Health Coverage
- OOP:
-
Out-of-Pocket Payment
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
- WHO:
-
World Health Organization
References
WHO, Bank W. Global Monitoring Report on Financial Protection in Health 2019. 2019.
Chukwuemeka A, Umeh, Feeley FG. Inequitable Access to Health Care by the Poor in Community-Based Health Insurance Programs: A Review of Studies From Low- and Middle-Income Countries. Global Health: Science and Practice 2017, 5.
Wagstaff A, Flores G, Hsu J, Smitz M-F, Chepynoga K, Buisman LR, van Wilgenburg K, Eozenou P. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Global Health. 2018;6:e169–79.
Voorhoeve A, Ottersen T, Norheim OF. Making fair choices on the path to universal health coverage: a précis. Health Econ Policy Law. 2016;11:71–7.
FMOH. Ethiopia health accounts, 2013/2014. Addis Ababa, Ethiopia; 2017.
Alebachew A, Yusuf Y, Mann C, Berman P. Ethiopia’s Progress in health financing and the contribution of the 1998 health care and financing strategy in Ethiopia. MA, Addis Ababa: Harvard TH Chan School of Public Health and Breakthrough International Consultancy, PLC 2015, 95.
FMOH. Evaluation of community-based health insurance pilot schemes in Ethiopia: final report. Addis Ababa: Ethiopian Health Insurance Agency; 2015.
Ali EE. Health care financing in Ethiopia: implications on access to essential medicines. Value Health Reg Issues. 2014;4 C:37–40.
Solomon Feleke W, Mitiku H, Zelelew, Ashagari TD. Ethiopia’s Community-based health insurance: A step on the road to universal health coverage. Health Finance & Governance; 2014.
Tesfay G. The impact of community-based health insurance in health service utilization in Tigray; (Case of Kilte Awlaelo woreda. Mekelle, 2014.
Darius Erlangga M, Suhrcke S, Ali, Bloor K. The impact of public health insurance on health care utilization, financial protection, and health status in low- and middle-income countries: A systematic review. PLoS ONE 2019, 14.
Alebachew A, Yusuf Y, Mann C, Berman P. FMOH: Ethiopia’s progress in health financing and the contribution of the 1998 health care and financing strategy in Ethiopia. (Project. RTaM ed. Boston, Massachusetts and addis Ababa, Ethiopia: Harvard T.H. Chan school of public health. Breakthrough International Consultancy, PLC; and Ethiopian Federal Ministry of Health; 2015.
Kasim Ebrahim F, Yonas, Kaso M. Willingness of community to enroll in community-based health insurance and associated factors at household level in Siraro district, West Arsi zone, Ethiopia. J Public Health Epidemiol August. 2019;11:137–44.
Melaku Haile S, Ololo, Megersa B. Willingness to join community-based health insurance among rural households of debub bench district, bench Maji zone, Southwest Ethiopia. BMC Public Health 2014, 14.
Dawit Nageso K, Tefera, Gutema K. Enrollment in community-based health insurance program and the associated factors among households in Boricha district, Sidama zone, Southern Ethiopia; a cross-sectional study. PLoS ONE 2020, 15.
Alem Deksisa M, Abdo E, Mohamed D, Tolesa S, Garoma A, Zewdie M, Lami D, Irena D, Abdena. Lemi1 H: willingness of community-based health insurance uptake and associated factors among urban residents of oromia regional State, oromia, Ethiopia, a cross-sectional study. BMC Health Serv Res 2020, 20.
Asaye AW, MT E. Determinants of Community Based Health Insurance Implementation: Evidence from South Gondar Zone, Amhara Region (2020). Journal of Women’s Health Care 2020, 10.
Atafu A, Kwon S. Adverse selection and supply-side factors in the enrollment in community‐based health insurance in Northwest Ethiopia: A mixed methodology. Int J Health Plann Manag. 2018;33:902–14.
Berhanu Bifato A, Ayele M, Rike, Dangura D. Community based health insurance enrollment and associated factors in Sidama region, Ethiopia. J Trop Disease Public Health. 2021;9:297.
Biset Wagaw G, Tadesse AW, Ambaye GY. Willingness to join community-based health insurance among households in South Wollo, Northeast Ethiopia: A community-based cross-sectional study. PLoS ONE. 2022;17:e0261642.
Dibaba TJ, Terefa DR, BW H. Willingness to join Community-Based health insurance and its predictors among informal sectors in Buno Bedele zone, South West Ethiopia. Int J Health Econ Policy. 2021;6:118–26.
Dojamo T. Determinants of enrollment to community-based health insurance among rural households in Jimma zone, Southwest Ethiopia: Case-control study. Jimma University; 2018.
Geferso AT, Sharo SB. Community-Based Health Insurance Utilization and Its Associated Factors among Rural Households in Akaki District, Oromia, Ethiopia, 2021. Advances in Public Health 2022, 2022:9280269.
Minyihun A, Assefa Y, Debie A, Amare G. Willingness to join Community-Based health insurance among rural households of Bugna district, Northeast Ethiopia. Ethiop J Health Biomedical Sci. 2020;10:35–45.
Mulugeta Mekuria, Girma T. Community-based Health Insurance Coverage, Drop-out Rates and Associated Factors Among Households in Selected Districts of West Shewa Zone, Ethiopia. Ambo, Department of Public Health; 2020.
Abdilwohab MG, Abebo ZH, Godana W, Ajema D, Yihune M, Hassen H. Factors affecting enrollment status of households for community-based health insurance in a resource-limited peripheral area in Southern Ethiopia. Mixed method. PLoS ONE 2021, 16.
Taddesse G, Atnafu DD, Ketemaw A, Alemu Y. Determinants of enrollment decision in the community-based health insurance, North West Ethiopia: a case-control study. Globalization Health. 2020;16:1–9.
Yitayew MY, Adem MH, NS T. Willingness to enroll for Community-Based health insurance and associated factors in Simada district, North-West, Ethiopia, 2020: A Community-Based Cross-Sectional study. Risk Manage Healthc Policy. 2020;13:3031.
Shibeshi S. Assessment of factors affecting uptake of community-based health insurance among Sabata Hawas woreda community, Oromiya region. Addis Ababa University; 2017.
Kebede A, Gebreslassie M, Yitayal M. Willingness to enroll for community-Based health insurance and associated factors among household heads in the rural community of Fogera district, Northwest Ethiopia. Ethiop J Health Biomedical Sci. 2020;10:13–20.
Dejenu Kibret G, Tesema Leshargie CH, Fasil Wagnew, Alebel A. Willingness to join community-based health insurance and its determinants in East Gojjam zone, Northwest Ethiopia. BMC Res Notes 2019, 12.
Fite MB, Roba KT, Merga BT, Tefera BN, Beha GA, TT G. Factors associated with enrollment for community-based health insurance scheme in Western Ethiopia: Case-control study. PLoS ONE. 2021;16:e0252303.
Mulugeta Mekuria T, Benti, Chaka EE. Willingness to join Community-Based health insurance and factors affect it among households of selected districts of West Shoa zone, Ethiopia: A Community-Based Cross-Sectional study. J Health Med Nurs 2019, 65.
Garedew MG, Sinkie SO, Handalo DM. Waju Beyene Salgedo, Kidus Yitebarek Kehali, Feyera Gebissa Kebene, Tesfaye Dagne waldemarium, Mengesha MA: willingness to join and pay for Community-Based health insurance among rural households of selected districts of Jimma zone, Southwest Ethiopia. ClinicoEconomics Outcomes Res. 2020;12:45–55.
Negash B, Dessie Y, Gobena T. Community based health insurance utilization and associated factors among informal workers in Gida Ayana district, oromia region, West Ethiopia. East Afr J Health Biomedical Sci. 2019;3:13–22.
Asmamaw Atnafu, Tariku A. Perceived quality of healthcare and availability of supplies determine Household-Level willingness to join a Community-Based health insurance scheme in Amhara region, Ethiopia. ClinicoEconomics Outcomes Res. 2020;12:683–91.
Elmi A, Oladeji O, Robins A, Tahir A. Determinants of enrolment for community based health insurance scheme among Agro-pastoralist communities of Aw-barre district in the Somali region of Ethiopia: unmatched case-control study. 2021.
Tadesse F. Assessment of the current community-based health insurance utilization and the associated factors in the community of Bole sub-city, addis Ababa, Ethiopia. Addis Continental Institute of Public Health; 2021.
Mirach TH, Demissie GD, Biks GA. Determinants of community-based health insurance implementation in West Gojjam zone, Northwest Ethiopia: a community-based cross-sectional study design. BMC Health Serv Res 2019, 19.
Tahir A, Abdilahi AO, Farah AE. Pooled coverage of community-based health insurance scheme enrolment in Ethiopia, systematic review and meta-analysis, 2016–2020. Health Econ Rev. 2022;12:38.
Eseta WA, Lemma TD, Geta ET. Magnitude and determinants of dropout from Community-Based health insurance among households in Manna district, Jimma zone, Southwest Ethiopia. ClinicoEconomics Outcomes Res. 2020;12:747–60.
Birhanu Ashagrie GA, Biks, Belew AK. Community-Based health insurance membership dropout rate and associated factors in dera district, Northwest Ethiopia. Risk Manage Healthc Policy. 2020;13:2835–44.
Workneh SG, Biks GA, Woreta SA. Community-based health insurance and communities’ scheme requirement compliance in Thehuldere district, Northeast Ethiopia: cross-sectional community-based study. ClinicoEconomics Outcomes Res 2017:353–9.
Simieneh MM, Yitayal M, Gelagay AA. Effect of community-based health insurance on healthcare-seeking behavior for childhood illnesses among rural mothers in aneded district, East Gojjam zone, Amhara region, Northwest Ethiopia. Risk Manage Healthc Policy 2021:1659–68.
Atnafu A, Gebremedhin T. Community-based health insurance enrollment and child health service utilization in Northwest Ethiopia: a cross-sectional case comparison study. ClinicoEconomics Outcomes Res 2020:435–44.
Gebru T, Lentiro K. The impact of community-based health insurance on health-related quality of life and associated factors in Ethiopia: a comparative cross-sectional study. Health Qual Life Outcomes. 2018;16:1–6.
Habte A, Tamene A, Ejajo T, Dessu S, Endale F, Gizachew A, Sulamo D. Towards universal health coverage: the level and determinants of enrollment in the Community-Based health insurance (CBHI) scheme in Ethiopia: A systematic review and meta-analysis. PLoS ONE. 2022;17:e0272959.
Moher D, Liberati A, Tetzlaff J, DG A, Group TP. Preferred reporting items for systematic reviews and Meta-Analyses: the PRISMA statement. PLoS Med 2009, 6.
Porritt K, Gomersall J, Lockwood C. JBI’s systematic reviews: study selection and critical appraisal. AJN Am J Nurs. 2014;114:47–52.
Farrah K, Young K, Tunis MC, Zhao L. Risk of bias tools in systematic reviews of health interventions: an analysis of PROSPERO-registered protocols. Syst Reviews. 2019;8:1–9.
Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manage. 2014;3:123.
Institute JB. The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews. Critical Appraisal Checklist for Cohort Studies; 2017.
Cohen JF, Chalumeau M, Cohen R, Korevaar DA, Khoshnood B, Bossuyt PM. Cochran’s Q test was useful to assess heterogeneity in likelihood ratios in studies of diagnostic accuracy. J Clin Epidemiol. 2015;68:299–306.
von Hippel PT. The heterogeneity statistic I 2 can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15:1–8.
Chanie MG, Ewunetie GE. Determinants of enrollment in community-based health insurance among households in Tach-Armachiho woreda, North Gondar, Ethiopia, 2019. PLoS ONE. 2020;15:e0236027.
Molla A. N F: Predictors of willingness to participate in health insurance services among the community of Jimma town, Southwest Ethiopia. Health Serv Insights 2014, 7.
Alegn T. Determinants of participation in a Community-Based health insurance scheme in Bambasi woreda. Benishangul Gumuz Region. Addis Ababa University; 2019.
Oriakhi H. E Onemolease 2012 Determinants of rural household’s willingness to participate in community-based health insurance scheme in Edo State, Nigeria. Stud ethno-medicine 6 95–102.
Maina JM, Kithuka P, Tororei S. Perceptions and uptake of health insurance for maternal care in rural Kenya: a cross-sectional study. Pan Afr Med J 2016, 23.
Cheno RW, Tchabo W, Tchamy J. Willingness to join and pay for community-based health insurance and associated determinants among urban households of Cameroon: a case of Douala and Yaounde. Heliyon 2021, 7.
Nshakira-Rukundo E, Mussa EC, Nshakira N, Gerber N, Von Braun J. Determinants of enrolment and renewing of community-based health insurance in households with under-5 children in rural south-western Uganda. Int J Health Policy Manage. 2019;8:593.
Otieno PO, Wambiya EOA, Mohamed SF, Donfouet HPP, Mutua MK. Prevalence and factors associated with health insurance coverage in resource-poor urban settings in Nairobi, Kenya: a cross-sectional study. BMJ Open. 2019;9:e031543.
Ko H, Kim H, Yoon C-g. Kim C-y: social capital as a key determinant of willingness to join community-based health insurance: a household survey in Nepal. Public Health. 2018;160:52–61.
Gobir A, Adeyemi A, Abubakar A, Audu O, Joshua I. Determinants of willingness to join community-Based health insurance scheme in a rural community of North-Western Nigeria. Afr J Health Econ. 2016;5:1–10.
Oluedo E, Obikeze E, Nwankwo C, Okonronkwo I. Willingness to enroll and pay for community-based health insurance, decision motives, and associated factors among rural households in Enugu State, Southeast Nigeria. Niger J Clin Pract. 2023;26:908–20.
Esther F, Adebayo OA, Uthman CS, Wiysonge EA, Stern, Kim T, Lamont, Ataguba JE. A systematic review of factors that affect the uptake of community-based health insurance in low-income and middle-income countries. BMC Health Serv Res 2015, 15.
Racha Fadlallah F, El-Jardali N, Hemadi RZ, Morsi. Clara Abou Abou Samra, Ali Ahmad, Khurram Arif, Lama Hishi, Gladys Honein-AbouHaidar, Akl EA: Barriers and facilitators to implementation, uptake and sustainability of community-based health insurance schemes in low and middle-income countries: a systematic review. International Journal for Equity in Health (2018) 17:13 2018, 17.
Dror DM, Hossain SS, Majumdar A, Pérez Koehlmoos TL, John D, Panda PK. What factors affect voluntary uptake of community-based health insurance schemes in low-and middle-income countries? A systematic review and meta-analysis. PLoS ONE. 2016;11:e0160479.
Shewamene Z, Tiruneh G, Abraha A, Reshad A, Terefe MM, Shimels T, Lemlemu E, Tilahun D, Wondimtekahu A, Argaw M, et al. Barriers to uptake of community-based health insurance in sub-Saharan Africa: a systematic review. Health Policy Plann. 2021;36:1705–14.
Bayked EM, Kahissay MH, Workneh BD. Factors affecting the uptake of community-based health insurance in Ethiopia: a systematic review. Int J. 2021;7:459.
Shewamene Z, Tiruneh G, Abraha A, Reshad A, Terefe MM, Shimels T, Lemlemu E, Tilahun D, Wondimtekahu A, Argaw M. Barriers to uptake of community-based health insurance in sub-Saharan Africa: a systematic review. Health Policy Plann. 2021;36:1705–14.
Acknowledgements
We would like to acknowledge the authors of the primary studies.
Funding
No specific funding was received for this analysis.
Author information
Authors and Affiliations
Contributions
Abdene Weya Kaso prepared the protocol for registration in PROSPERO, conceived the idea, and designed the study. Abdene Weya Kaso, Daniel Sisay, Berhanu Gidisa Debela, Helen Ali Ewune, and Habtamu Endashaw Hareru participated in database searching, data abstraction, and statistical analysis. Abdene Weya Kaso, Mary Abera Debisa, Habtamu Endashaw Hareru, and Alemayehu Hailu performed report writing and manuscript drafting. All the authors read and approved the final version of the manuscript before being considered for publication.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethical consent
NA
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kaso, A.W., Debela, B.G., Hareru, H.E. et al. Willingness to join community-based health insurance and associated factors among households in Ethiopian: a systematic review and meta-analysis. Cost Eff Resour Alloc 23, 12 (2025). https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12962-025-00620-0
Received:
Accepted:
Published:
DOI: https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s12962-025-00620-0